Introduction to Psychology

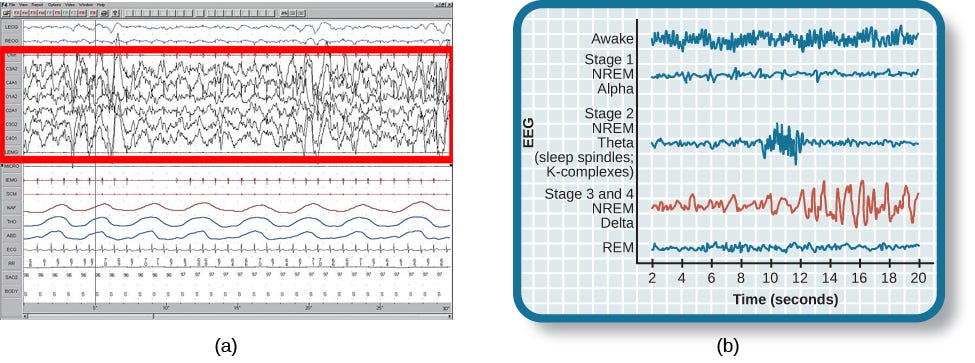
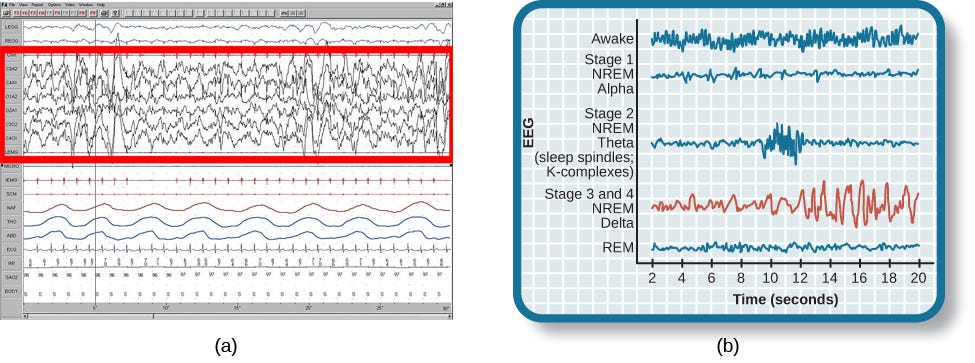
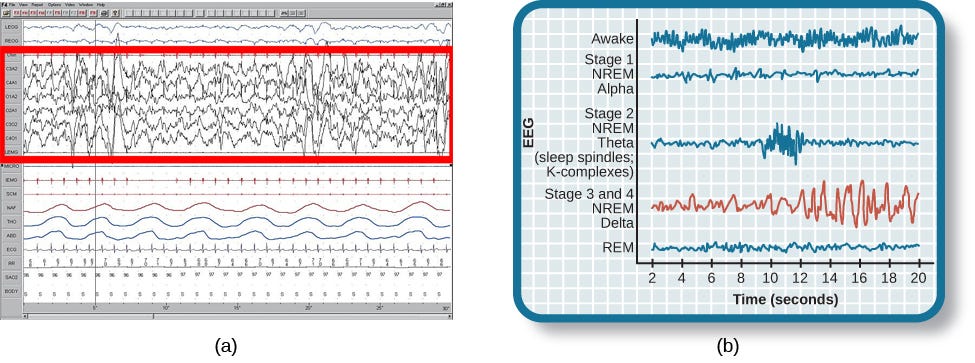
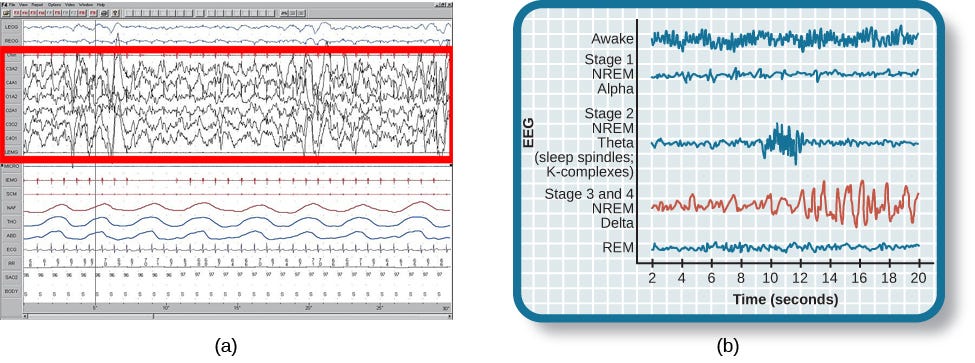
Sleep is not a uniform state of being. Instead, sleep is composed of several different stages that can be differentiated from one another by the patterns of brain wave activity that occur during each stage. These changes in brain wave activity can be visualized using EEG and are distinguished from one another by both the frequency and amplitude of brain waves . Sleep can be divided into two different general phases: REM sleep and non-REM (NREM) sleep. Rapid eye movement (REM) sleep is characterized by darting movements of the eyes under closed eyelids. Brain waves during REM sleep appear very similar to brain waves during wakefulness. In contrast, non-REM (NREM) sleep is subdivided into four stages distinguished from each other and from wakefulness by characteristic patterns of brain waves. The first four stages of sleep are NREM sleep, while the fifth and final stage of sleep is REM sleep. In this section, we will discuss each of these stages of sleep and their associated patterns of brain wave activity.
NREM STAGES OF SLEEP
The first stage of NREM sleep is known as stage 1 sleep. Stage 1 sleep is a transitional phase that occurs between wakefulness and sleep, the period during which we drift off to sleep. During this time, there is a slowdown in both the rates of respiration and heartbeat. In addition, stage 1 sleep involves a marked decrease in both overall muscle tension and core body temperature.
In terms of brain wave activity, stage 1 sleep is associated with both alpha and theta waves. The early portion of stage 1 sleep produces alpha waves, which are relatively low frequency (8–13Hz), high amplitude patterns of electrical activity (waves) that become synchronized . This pattern of brain wave activity resembles that of someone who is very relaxed, yet awake. As an individual continues through stage 1 sleep, there is an increase in theta wave activity. Theta waves are even lower frequency (4–7 Hz), higher amplitude brain waves than alpha waves. It is relatively easy to wake someone from stage 1 sleep; in fact, people often report that they have not been asleep if they are awoken during stage 1 sleep.
As we move into stage 2 sleep, the body goes into a state of deep relaxation. Theta waves still dominate the activity of the brain, but they are interrupted by brief bursts of activity known as sleep spindles . A sleep spindle is a rapid burst of higher frequency brain waves that may be important for learning and memory (Fogel & Smith, 2011; Poe, Walsh, & Bjorness, 2010). In addition, the appearance of K-complexes is often associated with stage 2 sleep. A K-complex is a very high amplitude pattern of brain activity that may in some cases occur in response to environmental stimuli. Thus, K-complexes might serve as a bridge to higher levels of arousal in response to what is going on in our environments (Halász, 1993; Steriade & Amzica, 1998).
Stage 3 and stage 4 of sleep are often referred to as deep sleep or slow-wave sleep because these stages are characterized by low frequency (up to 4 Hz), high amplitude delta waves . During this time, an individual’s heart rate and respiration slow dramatically. It is much more difficult to awaken someone from sleep during stage 3 and stage 4 than during earlier stages. Interestingly, individuals who have increased levels of alpha brain wave activity (more often associated with wakefulness and transition into stage 1 sleep) during stage 3 and stage 4 often report that they do not feel refreshed upon waking, regardless of how long they slept (Stone, Taylor, McCrae, Kalsekar, & Lichstein, 2008).
REM SLEEP
As mentioned earlier, REM sleep is marked by rapid movements of the eyes. The brain waves associated with this stage of sleep are very similar to those observed when a person is awake., and this is the period of sleep in which dreaming occurs. It is also associated with paralysis of muscle systems in the body with the exception of those that make circulation and respiration possible. Therefore, no movement of voluntary muscles occurs during REM sleep in a normal individual; REM sleep is often referred to as paradoxical sleep because of this combination of high brain activity and lack of muscle tone. Like NREM sleep, REM has been implicated in various aspects of learning and memory (Wagner, Gais, & Born, 2001), although there is disagreement within the scientific community about how important both NREM and REM sleep are for normal learning and memory (Siegel, 2001).
If people are deprived of REM sleep and then allowed to sleep without disturbance, they will spend more time in REM sleep in what would appear to be an effort to recoup the lost time in REM. This is known as the REM rebound, and it suggests that REM sleep is also homeostatically regulated. Aside from the role that REM sleep may play in processes related to learning and memory, REM sleep may also be involved in emotional processing and regulation. In such instances, REM rebound may actually represent an adaptive response to stress in nondepressed individuals by suppressing the emotional salience of aversive events that occurred in wakefulness (Suchecki, Tiba, & Machado, 2012).
While sleep deprivation in general is associated with a number of negative consequences (Brown, 2012), the consequences of REM deprivation appear to be less profound (as discussed in Siegel, 2001). In fact, some have suggested that REM deprivation can actually be beneficial in some circumstances. For instance, REM sleep deprivation has been demonstrated to improve symptoms of people suffering from major depression, and many effective antidepressant medications suppress REM sleep (Riemann, Berger, & Volderholzer, 2001; Vogel, 1975).
It should be pointed out that some reviews of the literature challenge this finding, suggesting that sleep deprivation that is not limited to REM sleep is just as effective or more effective at alleviating depressive symptoms among some patients suffering from depression. In either case, why sleep deprivation improves the mood of some patients is not entirely understood (Giedke & Schwärzler, 2002). Recently, however, some have suggested that sleep deprivation might change emotional processing so that various stimuli are more likely to be perceived as positive in nature (Gujar, Yoo, Hu, & Walker, 2011). The hypnogram below shows a person’s passage through the stages of sleep.

Dreams
The meaning of dreams varies across different cultures and periods of time. By the late 19th century, German psychiatrist Sigmund Freud had become convinced that dreams represented an opportunity to gain access to the unconscious. By analyzing dreams, Freud thought people could increase self-awareness and gain valuable insight to help them deal with the problems they faced in their lives. Freud made distinctions between the manifest content and the latent content of dreams. Manifest content is the actual content, or storyline, of a dream. Latent content, on the other hand, refers to the hidden meaning of a dream. For instance, if a woman dreams about being chased by a snake, Freud might have argued that this represents the woman’s fear of sexual intimacy, with the snake serving as a symbol of a man’s penis.
Freud was not the only theorist to focus on the content of dreams. The 20th century Swiss psychiatrist Carl Jung believed that dreams allowed us to tap into the collective unconscious. The collective unconscious, as described by Jung, is a theoretical repository of information he believed to be shared by everyone. According to Jung, certain symbols in dreams reflected universal archetypes with meanings that are similar for all people regardless of culture or location.
The sleep and dreaming researcher Rosalind Cartwright, however, believes that dreams simply reflect life events that are important to the dreamer. Unlike Freud and Jung, Cartwright’s ideas about dreaming have found empirical support. For example, she and her colleagues published a study in which women going through divorce were asked several times over a five month period to report the degree to which their former spouses were on their minds. These same women were awakened during REM sleep in order to provide a detailed account of their dream content. There was a significant positive correlation between the degree to which women thought about their former spouses during waking hours and the number of times their former spouses appeared as characters in their dreams (Cartwright, Agargun, Kirkby, & Friedman, 2006). Recent research (Horikawa, Tamaki, Miyawaki, & Kamitani, 2013) has uncovered new techniques by which researchers may effectively detect and classify the visual images that occur during dreaming by using fMRI for neural measurement of brain activity patterns, opening the way for additional research in this area.
Recently, neuroscientists have also become interested in understanding why we dream. For example, Hobson (2009) suggests that dreaming may represent a state of protoconsciousness. In other words, dreaming involves constructing a virtual reality in our heads that we might use to help us during wakefulness. Among a variety of neurobiological evidence, John Hobson cites research on lucid dreams as an opportunity to better understand dreaming in general. Lucid dreams are dreams in which certain aspects of wakefulness are maintained during a dream state. In a lucid dream, a person becomes aware of the fact that they are dreaming, and as such, they can control the dream’s content (LaBerge, 1990).
Summary
The different stages of sleep are characterized by the patterns of brain waves associated with each stage. As a person transitions from being awake to falling asleep, alpha waves are replaced by theta waves. Sleep spindles and K-complexes emerge in stage 2 sleep. Stage 3 and stage 4 are described as slow-wave sleep that is marked by a predominance of delta waves. REM sleep involves rapid movements of the eyes, paralysis of voluntary muscles, and dreaming. Both NREM and REM sleep appear to play important roles in learning and memory. Dreams may represent life events that are important to the dreamer. Alternatively, dreaming may represent a state of protoconsciousness, or a virtual reality, in the mind that helps a person during consciousness.

Glossary

alpha wave type of relatively low frequency, relatively high amplitude brain wave that becomes synchronized; characteristic of the beginning of stage 1 sleep

delta wave type of low frequency, high amplitude brain wave characteristic of stage 3 and stage 4 sleep

collective unconscious theoretical repository of information shared by all people across cultures, as described by Carl Jung
K-complex very high amplitude pattern of brain activity associated with stage 2 sleep that may occur in response to environmental stimuli

latent content hidden meaning of a dream, per Sigmund Freud’s view of the function of dreams

lucid dream people become aware that they are dreaming and can control the dream’s content

manifest content storyline of events that occur during a dream, per Sigmund Freud’s view of the function of dreams

non-REM (NREM) period of sleep outside periods of rapid eye movement (REM) sleep

rapid eye movement (REM) sleep period of sleep characterized by brain waves very similar to those during wakefulness and by darting movements of the eyes under closed eyelids

sleep spindle rapid burst of high frequency brain waves during stage 2 sleep that may be important for learning and memory
stage 1 sleep first stage of sleep; transitional phase that occurs between wakefulness and sleep; the period during which a person drifts off to sleep

stage 2 sleep second stage of sleep; the body goes into deep relaxation; characterized by the appearance of sleep spindles
stage 3 sleep third stage of sleep; deep sleep characterized by low frequency, high amplitude delta waves
stage 4 sleep fourth stage of sleep; deep sleep characterized by low frequency, high amplitude delta waves
type of low frequency, low amplitude brain wave characteristic of the end of stage 1 sleep
Sleep is a vital indicator of overall health and well-being. We spend up to one-third of our lives asleep, and the overall state of our “sleep health” remains an essential question throughout our lifespan
Most of us know that getting a good night’s sleep is important, but too few of us actually make those eight or so hours between the sheets a priority. For many of us with sleep debt, we’ve forgotten what “being really, truly rested” feels like.
To further complicate matters, stimulants like coffee and energy drinks, alarm clocks, and external lights — including those from electronic devices — interferes with our “circadian rhythm” or natural sleep/wake cycle.
Sleep needs vary across ages and are especially impacted by lifestyle and health. To determine how much sleep you need, it’s important to assess not only where you fall on the “sleep needs spectrum,” but also to examine what lifestyle factors are affecting the quality and quantity of your sleep such as work schedules and stress.
To get the sleep you need, you must look at the big picture.
How Much Sleep Do We Really Need: Revisited
The National Sleep Foundation released the results of a world-class study that took more than two years of research to complete — an update to our most-cited guidelines on how much sleep you really need at each age.
Eighteen leading scientists and researchers were tasked with updating the official sleep recommendations. The panelists included six sleep specialists and representatives from leading organizations including the American Academy of Pediatrics, American Association of Anatomists, American College of Chest Physicians, American Congress of Obstetricians and Gynecologists, American Geriatrics Society, American Neurological Association, American Physiological Society, American Psychiatric Association, American Thoracic Society, Gerontological Society of America, Human Anatomy and Physiology Society, and Society for Research in Human Development. The panelists participated in a rigorous scientific process that included reviewing over 300 current scientific publications and voting on how much sleep is appropriate throughout the lifespan.
How Much Sleep Do You Need?
Though research cannot pinpoint an exact amount of sleep need by people at different ages, our new chart, which features minimum and maximum ranges for health as well as “recommended” windows, identifies the “rule-of-thumb” amounts experts agree upon.
Nevertheless, it’s important to pay attention to your own individual needs by assessing how you feel on different amounts of sleep.
- Are you productive, healthy and happy on seven hours of sleep? Or does it take you nine hours of quality ZZZs to get you into high gear?
- Do you have health issues such as being overweight? Are you at risk for any disease?
- Are you experiencing sleep problems?
- Do you depend on caffeine to get you through the day?
- Do you feel sleepy when driving?
These are questions that must be asked before you can find the number that works for you.
Sleep Time Recommendations: What’s Changed?
A new range, “may be appropriate,” has been added to acknowledge the individual variability in appropriate sleep durations. The recommendations now define times as either (a) recommended; (b) may be appropriate for some individuals; or © not recommended.
The panel revised the recommended sleep ranges for all six children and teen age groups. A summary of the new recommendations includes:
- Newborns (0–3 months): Sleep range narrowed to 14–17 hours each day (previously it was 12–18)
- Infants (4–11 months): Sleep range widened two hours to 12–15 hours (previously it was 14–15)
- Toddlers (1–2 years): Sleep range widened by one hour to 11–14 hours (previously it was 12–14)
- Preschoolers (3–5): Sleep range widened by one hour to 10–13 hours (previously it was 11–13)
- School age children (6–13): Sleep range widened by one hour to 9–11 hours (previously it was 10–11)
- Teenagers (14–17): Sleep range widened by one hour to 8–10 hours (previously it was 8.5–9.5)
- Younger adults (18–25): Sleep range is 7–9 hours (new age category)
- Adults (26–64): Sleep range did not change and remains 7–9 hours
- Older adults (65+): Sleep range is 7–8 hours (new age category)
Improve Your Sleep Today: Make Sleep a Priority
To begin a new path towards healthier sleep and a healthier lifestyle, begin by assessing your own individual needs and habits. See how you respond to different amounts of sleep.
Pay careful attention to your mood, energy and health after a poor night’s sleep versus a good one. Ask yourself, “How often do I get a good night’s sleep?” Like good diet and exercise, sleep is a critical component to overall health.
To pave the way for better sleep, follow these simple yet effective healthy sleep tips, including:
- Stick to a sleep schedule, even on weekends.
- Practice a relaxing bedtime ritual.
- Exercise daily.
- Evaluate your bedroom to ensure ideal temperature, sound and light.
- Sleep on a comfortable mattress and pillows.
- Beware of hidden sleep stealers, like alcohol and caffeine.
- Turn off electronics before bed.
If you or a family member are experiencing symptoms such as sleepiness during the day or when you expect to be awake and alert, snoring, leg cramps or tingling, gasping or difficulty breathing during sleep, prolonged insomnia or another symptom that is preventing you from sleeping well, you should consult your primary care physician or find a sleep professional to determine the underlying cause.
Track your sleep habits over a one- or two-week period and bring the results to your physician.
Most importantly, make sleep a priority. You must schedule sleep like any other daily activity, so put it on your “to-do list” and cross it off every night. But don’t make it the thing you do only after everything else is done — stop doing other things so you get the sleep you need.
The Science Of Sleep —
When it comes to your health, sleep plays an important role. While more sleep won’t necessarily prevent you from getting sick, skimping on it could adversely affect your immune system, leaving you susceptible to a bad cold or case of the flu. To keep yourself sniffle-free this season, here’s what you need to know.
Sleep and Cytokines
Without sufficient sleep, your body makes fewer cytokines, a type of protein that targets infection and inflammation, effectively creating an immune response. Cytokines are both produced and released during sleep, causing a double whammy if you skimp on shut-eye. Chronic sleep loss even makes the flu vaccine less effective by reducing your body’s ability to respond.
Stock Up on Naps
To stay healthy, especially during the virus season, get the recommended seven to eight hours of sleep a night. This will help keep your immune system in fighting shape, and also protect you from other health issues including heart disease, diabetes, and obesity. If your sleep schedule is interrupted by a busy workweek or other factors, try to make up for the lost rest with naps. Taking two naps that are no longer than 30 minutes each — one in the morning and one in the afternoon — has been shown to help decrease stress and offset the negative effects that sleep deprivation has on the immune system. If you can’t swing a half-hour nap during the workday, try grabbing a 20-minute siesta on your lunch hour, and another right before dinner
Understanding sleep
Good sleep is necessary for physical and mental health. For example, sleep loss impairs immune function, and sleep is altered during infection. Immune signalling molecules are present in the healthy brain, where they interact with neurochemical systems to contribute to the regulation of normal sleep. Studies have shown that interactions between immune signalling molecules (such as the cytokine interleukin 1) and brain neurochemical systems (such as the serotonin system) are amplified during infection, indicating that these interactions might underlie the changes in sleep that occur during infection. Why should the immune system cause us to sleep differently when we are sick?
Alterations in sleep architecture during infection are exquisitely tailored to support the generation of fever, which in turn imparts survival value.
Modern sleep research began in 1953, with the discovery of rapid eye movement (REM) sleep and the realization that sleep is an active process that consists of two distinct phases. More than half a century of intense investigation has yet to provide an unequivocal answer to the question, ‘Why do we sleep?’ Nonetheless, we are beginning to understand the contribution of sleep to fundamental brain processes,.
In contrast to our lack of knowledge regarding the precise functions of sleep, we do know why we have an immune system. Living organisms are subject to constant attack by various pathogens, and the complex networks of physical and biochemical components that constitute the immune system keep the organism alive. Like sleep research, the field of immunology is a relatively young discipline. It should therefore not come as a surprise that systematic investigations of interactions between sleep and the immune system have only been conducted in the past 25 years (TIMELINE).
Although we briefly touch on the general role of sleep in health and disease, in this article we focus on those areas of research that are most relevant to sleep as a component of the host defence against microbial pathogens. Links between the CNS and the peripheral immune system are now well established, and much is known about the mechanisms by which bidirectional communication occurs between these systems. As a result of neuro-immune interactions, sleep loss alters immune function and immune challenges alter sleep. Thus, chronic sleep loss results in pathologies that are associated with increases in inflammatory mediators, and inflammatory mediators that are released during immune responses to infection alter CNS processes and behaviour, including sleep.
One class of immunomodulators, cytokines, has been extensively studied both with respect to host responses to infection and as regulators of physiological sleep. In here, we briefly summarize what is known about cytokines in the brain as regulators of normal, physiological sleep and what is known about their role in mediating the changes in sleep that are induced by infectious agents. We focus on one cytokine, interleukin 1 (IL-1), which, together with tumour necrosis factor (TNF), is the most investigated cytokine with respect to sleep. We then address the mechanisms by which IL-1 affects neurons and neurotransmitters involved in sleep regulation. Thus, the role of the serotonergic system in the regulation of sleep and as a mediator of IL-1’s effects on sleep is reviewed. The functional role of infection-induced alterations in sleep suggests the precise manner in which sleep is altered during infection facilitates the generation of fever and so promotes recovery.
Sleep in health and disease
Sleep is necessary for health
Although the brain gives us signals that indicate when we have had insufficient sleep, data show that more and more of us are ignoring these signals and reducing the amount of sleep we obtain each night. The percentage of adults who sleep less than 6 h per night is now greater than at any other time on record. These survey data do not allow us to determine the extent to which the declining amounts of sleep are due to sleep disorders or to behavioural decisions, but it is clear that our current practice of sleeping less is largely driven by societal changes, including increased reliance on longer work hours and shift work, the trend for longer commute times, and increased accessibility to media of all sorts.
What are the consequences of sleep loss? Historically, it was widely thought that the only consequence of nighttime sleep loss was daytime sleepiness resulting in cognitive impairment. We now have compelling evidence that, in addition to cognitive impairment, sleep loss is associated with a wide range of detrimental consequences, with tremendous public-health ramifications. For example, short periods of sleep loss at the time of vaccination reduce the vaccine’s effectiveness,. Sleep loss is associated with increased obesity,and with reduced levels of leptin and increased levels of ghrelin,, the combination of which increases appetite. Sleep loss is also associated with diabetes and impaired glucose tolerance in a dose-related manner: individuals that report sleeping less than 6 h per night are ~1.7 times as likely, and those that report sleeping less than 5 h per night are ~2.5 times as likely, to have diabetes than individuals that obtain 7 h of sleep. Cardiovascular disease and hypertension are also associated with sleep loss: the risk of a fatal heart attack increases 45% in individuals who chronically sleep 5 h per night or less. Collectively, these examples demonstrate wide- ranging consequences of sleep loss on physical health. Obesity, diabetes and cardiovascular disease are pathologies that are characterized, in part, by inflammatory processes. The magnitude of the public-health burden imposed by these and other diseases underscores the importance of relationships between sleep and immune function and our efforts to understand them.
Sleep is disturbed during disease
We have all experienced the feelings of lethargy and fatigue associated with being sick. Some infections induce dramatic alterations in sleep. For example, recent cases of an encephalitis lethargica-like syndrome have been associated with streptococcal infections, during which severe sleep disruption occurs. In addition, there is an extensive body of literature which demonstrates that the sleep of individuals infected with HIV is altered even before they show symptoms of AIDS. Furthermore, infection with the parasite Trypanosoma brucei, the causative agent of human African trypanosomiasis (sleeping sickness), results in extreme fragmentation of sleep and a complete loss of the diurnal rhythms of sleep and wakefulness,. Although most people fortunately do not encounter these catastrophic infections, we have all suffered colds or ‘the flu’, and sleep is altered during these more common infections as well,.
Cytokines and sleep
Immune responses during infection include alterations in the concentrations and patterns of immune signalling molecules called cytokines. The list of cytokines and chemokines that have been studied in laboratory animals or human subjects and demonstrated to affect sleep is extensive and includes IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-13, IL-15, IL-18, TNFα, TNFβ, interferon-α (IFNα), IFN-β, INF-γ and macrophage inhibitory protein 1β (also known as CCL4). Of these substances only two, IL-1β (hereafter referred to as IL-1) and TNFα (hereafter referred to as TNF), have been studied extensively enough to state that they are involved in the regulation of physiological (that is, spontaneous) sleep -. Evidence for a role for IL-1 and TNF in the regulation of physiological sleep has been derived from electrophysiological, biochemical and molecular genetic studies.
Cytokines participate in the regulation of sleep
Although most cytokines were first discovered in the peripheral immune system, several cytokines and their receptors have now been shown to be present in the CNS -. The CNS detects activation of the peripheral immune system through cytokine-induced stimulation of the vagus nerve, through actions of circulating cytokines at the cir-cumventricular organs and through active transport of cytokines from the periphery into the CNS (reviewed in REF. ). However, cytokines are also synthesized de novo and released in the CNS by both neurons -and glia. Neurons that are immunoreactive for IL-1 and TNF are located in brain regions that are implicated in the regulation of sleep-wake behaviour, notably the hypothalamus, the hippocampus and the brainstem,. Signalling receptors for both IL-1 and TNF are also present in several brain areas, such as the choroid plexus, the hippocampus, the hypothalamus, the brainstem and the cortex, and are expressed in both neurons and astrocytes,,.
IL-1 and TNF increase non-REM (NREM) sleep in several species (rat, mouse, monkey, cat, rabbit and sheep) irrespective of the route of administration,. NREM sleep that follows the administration of IL-1 or TNF has some characteristics of physiological sleep in the sense that it remains episodic and is easily reversible when the animal is stimulated. However, IL-1 generally causes fragmentation of NREM sleep. The magnitude and duration of IL-1’s effects on NREM sleep depend on the dose,and time,of administration: very high doses are NREM-sleep suppressive and, in rodents, IL-1 is more effective in increasing NREM sleep when it is administered before the dark phase of the light-dark cycle,.
In accordance with the increase in NREM sleep that occurs after administration of IL-1 or TNF, antagonizing either of these cytokine systems reduces spontaneous NREM sleep. For example, inactivating or interfering with the normal action of IL-1 or TNF by means of antibodies, antagonists or soluble receptors reduces both spontaneous NREM sleep and the increase in NREM sleep that occurs after sleep deprivation,. Preventing the cleavage of active IL-1 from its inactive precursor also reduces spontaneous NREM sleep. Furthermore, antagonizing these cytokine systems attenuates the increase in NREM sleep that follows excessive food intake or acute elevation of ambient temperature, both of which are associated with enhanced production of either IL-1 or TNF. Moreover, knockout mice that lack the type 1 IL-1 receptor, the type 1 TNF receptor or both spend less time in NREM sleep than control mice.
Administration of cytokines has been repeatedly shown to suppress REM sleep, but antagonizing endogenous cytokines in healthy animals with receptor antagonists, soluble receptors or antibodies either has no effect on REM sleep or only slightly reduces it,,. These observations suggest that cytokines modulate REM sleep during pathological conditions but do not contribute to the regulation of normal, physiological REM sleep. Moreover, recent demonstrations that alterations in REM sleep in mice lacking both IL-1 receptor 1 and TNF receptor 1 occur independently of changes in NREM sleep suggest that these cytokines influence REM sleep through mechanisms that differ from those that are involved in NREM-sleep regulation.
Finally, the fact that diurnal rhythms of IL-1 and TNF levels vary with the sleep-wake cycle provides further evidence for the involvement of IL-1 and TNF in physiological sleep regulation,. In rats, IL-1 and TNF mRNA and protein levels in the brain exhibit a diurnal rhythm with peaks that occur at light onset; the light period in these rodents is the time when NREM sleep propensity is at a maximum. In humans, IL-1 plasma levels are highest at the onset of sleep, and in cats cerebrospinal fluid IL-1 levels vary with the sleep-wake cycle.
Cytokines mediate changes in sleep induced by infection
The data briefly reviewed above show that at least two pro-inflammatory cytokines are involved in regulating spontaneous, physiological NREM sleep. The question that then arises is whether these cytokines also mediate infection-induced alterations in sleep. Numerous systematic preclinical studies have demonstrated the extent to which infection alters sleep (reviewed in REFS ,,). Although the precise alterations depend on the pathogen (bacteria, viruses, fungi or parasites), the host and the route of infection, at some time during the course of most infections there is an increase in the amount of time spent in NREM sleep and a decrease in the amount of REM sleep.
Models in which replicating pathogens are used to make animals sick are the most clinically relevant, but these types of studies are difficult to perform and interpret because the disease state develops over periods of days to weeks and the responsiveness to the infection can differ dramatically between animals. However, the changes induced in sleep by infectious agents are due to immune responses to biologically active structural components of the pathogen. Indeed, administration of such biologically active structural components results in changes in sleep that mimic those observed during infection with replicating pathogens. For this reason, most mechanistic studies of infection-induced alterations in sleep have used these structural components to induce the many facets of immune responses in the absence of replicating pathogens. The most commonly used are bacterial cell wall components such as lipid A, lipopolysaccharide and muramyl peptide (or the synthetic muramyl dipeptide). These bacterial cell wall components induce strong antigenic responses such as upregulation of pro-inflammatory cytokines, including IL-1 and TNF -. When these bacterial cell wall components are administered to rabbits, rats, mice or humans ( BOX 1), NREM sleep is increased and fragmented and REM sleep is suppressed.
Sleep and immunity in humans
There are some differences between laboratory animals and human subjects with respect to sleep-immune interactions. Most studies that use laboratory animals focus on the effects of host-defence activation on sleep and often include as outcome measures changes in immunomodulators in the brain. By contrast, the vast majority of studies that use human volunteers determine the effects of sleep loss on multiple facets of immunity, and immune-related outcome measures are almost always restricted to measures that can be obtained from whole blood, serum or plasma. The negative impact of sleep loss on public health is now recognized for pathologies that involve inflammatory processes, underscoring the importance of sleep to a healthy immune system.
It would be unethical to experimentally infect humans, but there are numerous clinical studies that describe the impact of HIV or trypanosome infection on sleep, all of which report that sleep is indeed altered. Healthy human volunteers under careful medical supervision have been subjected to host-defence activation by purified endotoxin, an immune challenge in which there are no replicating pathogens. These studies show that humans are more sensitive to endotoxin than are laboratory animals; in humans, slow-wave sleep (the equivalent of non-rapid eye movement sleep in animals) is increased across the night by very low, subpyrogenic doses of endotoxin (less than one-thousandth of the per-bodyweight dose that elicits sleep responses in rats). As the endotoxin dose increases there are transient increases in slow-wave sleep, lasting approximately 1 h. With even higher doses of endotoxin a much stronger host-defence response develops and, as in laboratory animals, sleep is severely disrupted. This is probably due, in part, to increased activity of the hypothalamic-pituitary-adrenal axis, which induces wakefulness and promotes arousal,.
As mentioned above, in contrast to the few reports of the effect of host-defence activation by endotoxin in humans, there have been numerous systematic studies in which human volunteers have been deprived of sleep and effects on immunity determined. The first study of the effects of sleep loss on immunity in humans seems to be that of Palmblad et al.. They demonstrated that 48 h of sleep deprivation reduced phytohaemagglutinin-induced DNA synthesis in lymphocytes, an effect that persisted for 5 days. This study was followed by more than 50 other studies that showed effects of sleep deprivation on the human immune system. By way of example, 64 h sleep deprivation is associated with alterations in many aspects of immunity, including leukocytosis, increased natural killer cell activity and increased counts of white blood cells, granulocytes and monocytes. According to recent reports, as little as 4 h of sleep loss in a controlled laboratory setting increases the production of interleukin 6 and tumour necrosis factor by monocytes — an effect that, bioinformatic analyses suggest, is mediated by the nuclear factor-κB inflammatory signalling pathway. The number and scope of studies of human sleep loss and immunity exceed that which can be summarized in this Review, and so for recent comprehensive reviews see REFS ,.
Of importance to this discussion, the effects of bacterial cell wall components on sleep are attenuated or blocked if cytokine systems are antagonized. For example, increases in NREM sleep after lipopolysaccharide or muramyl dipeptide administration are blocked if the IL-1 system is antagonized,. These data suggest that infection-induced alterations in sleep are mediated by cytokines such as IL-1 and TNF. They also show that administration of cytokines or pathogen components can serve as a model of infection-induced alterations in sleep. The advantages of such models are that responses occur on a timescale of hours rather than days or weeks, that many facets of immune and behavioural responses to infection are elicited, and that it is relatively easy to titrate the magnitude of the desired response.
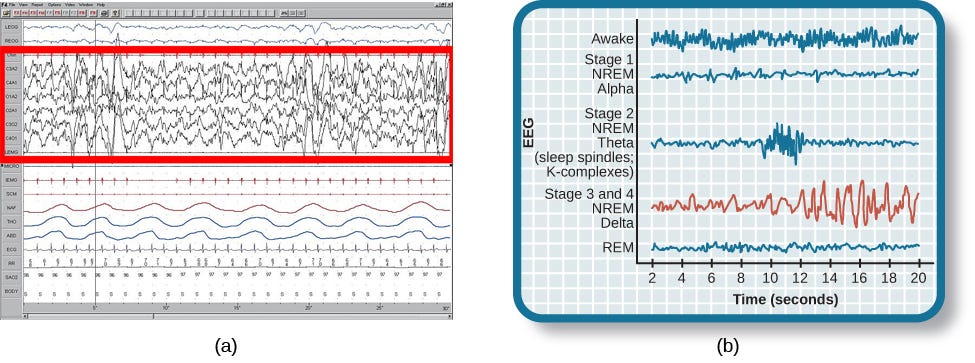
Serotonin and sleep
Sleep, like any behaviour, is regulated in the brain by multiple overlapping neuroanatomic circuits and related neurochemical systems. IL-1 and TNF interact with several of these systems, including the serotonin (also known as 5-hydroxytryptamine (5-HT)) system. The 5-HT system is one of the most investigated transmitter systems with respect to the regulation of sleep. In this section of the Review we briefly summarize the extensive body of literature that has demonstrated a role for the 5-HT system in regulating arousal states. Basic knowledge of 5-HT’s complex role in sleep regulation is necessary before one can fully understand how interactions between the IL-1 and 5-HT systems contribute to the regulation of sleep.
Observations in 1955 (REF. ) by Brodie and colleagues that brain 5-HT depletion by reserpine induces sedation prompted investigation of the role of 5-HT in the regulation of sleep-wake behaviour. 5-HT has since been shown to regulate multiple physiological processes and behaviours, including vigilance states, mood, food intake, thermoregulation, locomotion and sexual behaviour. The importance of the 5-HT system’s role in sleep regulation is supported by both experimental data and clinical observations: pharmacological manipulations that affect the 5-HT system by altering neurotransmitter synthesis, release, binding or re-uptake and metabolism result in profound alterations in sleep. Sleep is also altered during clinical conditions such as depression, in which the functionality of the 5-HT system is thought to be chronically altered.
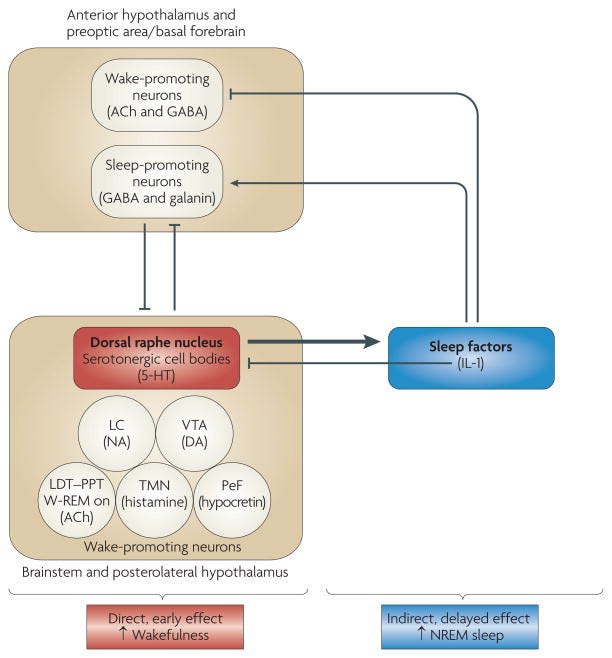
5-HT promotes arousal but is necessary for NREM sleep
The exact role of 5-HT in sleep regulation has been subject to debate,. Data obtained in the 1960s and early 1970s suggested that the 5-HT system is necessary for NREM sleep: the destruction of raphe nuclei (which contain the cell bodies of 5-HT neurons) or the depletion of brain 5-HT by administration of the 5-HT synthesis inhibitor p-chlorophenylalanine (PCPA) induces insomnia that is selectively reversed by the 5-HT precursor 5-hydroxytryptophan (5-HTP) ,. However, data obtained from the mid 1970s onwards suggested that 5-HT promotes wakefulness and suppresses NREM sleep. For instance, experimental manipulations that increase the release and synaptic availability of 5-HT, such as electrical stimulation of the dorsal raphe nuclei (DRN), enhance wakefulness, whereas DRN inactivation enhances sleep. In support of a wake-promoting role for 5-HT, a body of evidence has shown that the firing rates of serotonergic raphe neurons -and 5-HT release -are state-dependent: they peak during wakefulness and decrease during NREM sleep, and serotonergic cells become silent during REM sleep. In agreement with the interpretation that 5-HT is a wake-inducing substance, blockade of 5-HT 2 receptors increases NREM sleep in rats and humans. (A more detailed discussion of the role of 5-HT receptor subtypes in NREM-sleep regulation is beyond the scope of this Review.) 5-HT enhances wakefulness because serotonergic neurons in the DRN (together with other wake-promoting neurons, such as noradrenergic neurons in the brainstem locus coeruleus or hypocretinergic/orexinergic neurons in the hypothalamus) inhibit sleep-promoting neurons in the preoptic area, the anterior hypothalamus and the adjacent basal forebrain,(). Noradrenergic and hypocretinergic/orexinergic wake-promoting neurons also stimulate each other’s activity.
An attempt to integrate and reconcile these apparently contradictory data led to the hypothesis that 5-HT promotes wakefulness through direct actions and also stimulates the synthesis and/or release of sleep-promoting factors. Data now support this dual-role hypothesis for the involvement of 5-HT in the regulation of arousal states. The purported sleep-promoting factors induced by 5-HT drive sleep by inhibiting wake-promoting neurons and stimulating sleep-promoting neurons (). Data obtained from rats and mice -suggest that the role of 5-HT in the regulation of arousal states depends on the degree to which the 5-HT system is activated, the timing of the activation and the time that has passed since the activation (). When 5-HT release is enhanced in rats and mice through the administration of 5-HTP, the initial response is an increase in wakefulness and a reduction in NREM sleep -. This increase is fast, indicating that it is probably a direct effect of 5-HT. However, low doses of 5-HTP might not activate the 5-HT system sufficiently to stimulate sleep-inducing factors, a process that requires time. Following administration of higher physiological doses of 5-HTP, an increase in NREM sleep is apparent, after a delay, in both rats and mice -. This delayed increase in NREM sleep always occurs during the dark phase of the light-dark cycle, irrespective of the timing of 5-HTP administration -. Findings that 5-HTP administration increases the NREM sleep of rodents only during the dark phase suggest a fundamental property of the 5-HT system: the precise effects of serotonergic activation on sleep-wake behaviour depend not only on the extent but also on the timing of activation.
The data summarized above are in agreement with observations that acute administration in cats and rats of selective 5-HT re-uptake inhibitors first increases wake-fulness and then increases NREM sleep. The first studies of the relationship between 5-HT and sleep, carried out in the 1960s, were based on behavioural observations and did not include polygraphically defined determinations of vigilance states. Nevertheless, these studies reported biphasic responses to 5-HT administration in which behavioural ‘activation’ was followed by ‘depression’ (REF. ).
Serotonin suppresses REM sleep
Serotonergic neurons in the raphe nuclei, like noradrenergic neurons in the locus coeruleus, are considered to be part of the systems that gate REM sleep by inhibiting the neurons that promote it,. In this view, suppressed serotonergic activity is permissive of REM-sleep generation, which is consistent with observations that pharmacological inhibition of the 5-HT system enhances REM sleep whereas increases in synaptic 5-HT availability inhibit it. Accordingly, in rats and mice activation of the 5-HT system by administration of 5-HTP inhibits REM sleep, regardless of the dose and timing of administration -. The observation that mice that lack 5-HT 1A or 5-HT 1B receptor subtypes spend more time in REM sleep than control mice suggests that these receptor subtypes mediate the inhibitory effects of 5-HT on REM sleep. Such a conclusion, supported by responses to pharmacological blockade of the same receptor subtypes, of course does not rule out the possibility that 5-HT can also inhibit REM sleep by binding to other 5-HT receptor subtypes. At variance with the ‘REM-off’ role of 5-HT, observations that administration of a 5-HT 7 receptor antagonist inhibits REM sleep in rats and that 5-HT 7 receptor-knockout mice spend less time in this sleep phase suggest that 5-HT might have a facilitatory (or permissive) role in REM-sleep regulation through this specific receptor subtype. The role of 5-HT 2A or 5-HT 2C receptors in REM-sleep regulation is more complex.
Interactions between IL-1 and 5-HT
Evidence consistently demonstrates that IL-1 has a role in regulating physiological NREM sleep by acting, in part, through well-defined neuromodulatory systems. For example, IL-1 stimulates the synthesis and/or release of growth hormone-releasing hormone, prostaglandin D 2, adenosine and nitric oxide. Each of these substances is implicated in regulating or modulating NREM sleep, and antagonizing these systems attenuates or blocks IL-1-induced increases in NREM sleep. For an extensive review of the role of neuromodulatory systems in mediating cytokine effects on sleep, see REF. .
In addition to acting on these neuromodulatory systems, IL-1 acts directly on specific brain circuits and interacts with several neurotransmitters that have been implicated in regulating sleep. Thus, IL-1’s effects on NREM sleep could be mediated by actions on several neurotransmitter systems, although systematic investigations of the interactions between IL-1 and neurotransmitter systems that are relevant to the regulation of sleep remain to be conducted ( BOX 2). Here, we focus on the interactions between IL-1 and the 5-HT system because these are the interactions for which the most data have accumulated during the past 10 years. We review the evidence that IL-1 enhances NREM sleep in part through opposing but complementary actions on the 5-HT system in two distinct neuroanatomical regions, namely the DRN and the preoptic area of the hypothalamus, and the adjacent preoptic area and basal forebrain (POA/BF), which receives serotonergic innervation from the DRN. We show that IL-1 has inhibitory actions on the cell bodies of the wake-promoting DRN 5-HT system and increases 5-HT release from axon terminals in the POA/BF.
Effects of interleukin 1 on neurotransmitters involved in sleep regulation
This Rsection focuses on interactions between interleukin 1 (IL-1) and the serotonergic system and, where relevant, on interactions between IL-1 and the GABA (γ-aminobutyric acid)-ergic system. There are also some published reports of interactions between IL-1 and other neurotransmitter systems that are relevant to sleep regulation, and here we present a brief overview.
Acetylcholine (Ach)
Pontomesencephalic cholinergic neurons have a key role in rapid eye movement (REM) sleep generation and, together with basal forebrain cholinergic neurons, in cortical desynchronization and activation,. IL-1 inhibits ACh release in the hippocampus in vivo, inhibits ACh synthesis in vitro in cultured pituitary cells and increases acetylcholinesterase activity and mRNA expression in neuron-glia co-cultures and in vivo in the rat cortex. Suppression of REM sleep by IL-1 (REF. ) may be mediated by inhibition of pontomesencephalic cholinergic neurons.
Glutamate
Glutamate is widely used in the CNS. For instance, it is released by the neurons that project from the brainstem reticular formation, which is part of the ascending arousal system. Many anaesthetics attenuate glutamate-mediated neurotransmission. Interactions between IL-1 and glutamatergic neurotransmission have been investigated at length because of the involvement of glutamate excitotoxicity in neuron loss during stroke or chronic neurodegenerative disease. Evidence suggests that IL-1 can potentiate or inhibit the effects of glutamate,. For instance, IL-1 decreases evoked glutamatergic excitatory responses in hippocampal CA1 pyramidal neurons.
Adenosine
Adenosine, which is a by-product of energy metabolism, promotes sleep by inhibiting cholinergic and non-cholinergic wake-promoting neurons in the basal forebrain. Because IL-1 stimulates adenosine production,, this effect can further contribute to IL-1-induced increases in non-REM sleep. Moreover, IL-1-induced inhibition of glutamatergic responses (at least in the hippocampus) is mediated by adenosine.
Monoamines
Brainstem noradrenergic neurons of the locus coeruleus, dopaminergic neurons of the substantia nigra and ventral tegmental area and histaminergic neurons in the posterior hypothalamus are all wake-promoting. IL-1 activates these aminergic neurons and thereby enhances monoamine release in different brain areas. Owing to their role in promoting wakefulness, IL-1-induced activation of aminergic neurons might counteract the increase in NREM sleep and thus maintain homeostasis.
IL-1 actions in the DRN
IL-1 microinjection into the DRN of rats increases their NREM sleep. In a brainstem slice preparation, bath application of IL-1 reduces the firing rates of DRN wake-promoting serotonergic neurons,by enhancing GABA (γ-aminobutyric acid)-induced inhibitory postsynaptic potentials (). Thus, IL-1 potentiates the physiological GABAergic inhibition that shapes the state-dependent discharge of DRN serotonergic neurons. IL-1 potentiates GABA signalling through multiple mechanisms: it recruits GABA A receptors to the cell surface; it increases Cl −uptake by acting on GABA A receptors; and it induces a delayed potentiation of the GABA-elicited Cl −current, an effect that is suppressed by the IL-1 receptor antagonist. The observation that IL-1 potentiates the effects of GABA in the DRN is in agreement with data which demonstrate that IL-1 enhances GABA-induced hyperpolarization and inhibition in other brain regions where IL-1 acts both pre- and postsynaptically: IL-1 increases GABA release in anterior hypothalamic/pre-optic area slice preparations and in brain explants and enhances GABAergic inhibitory postsynaptic potentials in hippocampal neurons,.
IL-1 effects in the POA/BF
In the POA/BF, a brain area that is crucial for sleep regulation,, IL-1 directly inhibits wake-promoting neurons () and stimulates a subset of sleep-promoting neurons. IL-1 also increases the number of c-FOS-immunoreactive neurons in the POA/BF. The number of these c-FOS-immunoreactive neurons positively correlates with the amount of NREM sleep during the 2 h before sacrifice, suggesting that the stained neurons were active during this sleep phase and thus might be sleep-active neurons. In addition, IL-1 stimulates 5-HT release from axon terminals in the POA (). IL-1 induces a tonic increase in 5-HT release but does not alter the state-dependent pattern of release — that is, the phasic increases in 5-HT release during wakefulness and the decreases during sleep are superimposed on the tonic IL-1-induced increase in 5-HT release. The IL-1-induced enhancement of 5-HT release from axon terminals can result from local actions that are independent of the effects on serotonergic cell bodies in the DRN, because release from axon terminals is elicited by application of IL-1 directly into the hypothalamus. The POA/BF is the only brain area where increasing serotonergic activity by administering 5-HTP restores physiological sleep in cats that have been made insomniac by PCPA administration. 5-HT in the POA/BF might be essential for NREM sleep, because it hyperpolarizes and inhibits the cholinergic neurons that are responsible for cortical activation (). The results of these studies suggest that IL-1 stimulates NREM sleep in part by enhancing axonal 5-HT release in the POA/BF, where IL-1 and 5-HT inhibit wake-promoting neurons. 5-HT is essential for the effects of IL-1 on NREM sleep to fully manifest, because depletion of brain 5-HT by PCPA administration or blockade of 5-HT 2 receptors transiently interferes with IL-1-induced increases in NREM sleep.
Not only does IL-1 induce 5-HT release and inhibit wake-promoting neurons in the hypothalamus, but reciprocal interactions between the 5-HT system and the IL-1 system are also of importance. Increasing serotonergic activation with 5-HTP induces IL-1 mRNA transcription in the hypothalamus () during periods when NREM sleep is enhanced by the same treatment. There is specificity to this effect as 5-HTP does not alter IL-1 mRNA in the hippocampus or brainstem. The 5-HTP-induced increase in IL-1 mRNA may be part of a self-sustaining regulatory loop, because IL-1 induces its own synthesis,. As a consequence, IL-1 can amplify the 5-HTP-induced increase in IL-1 concentrations in the POA/BF, thus potentiating the inhibition of wake-promoting neurons in this region (). Finally, IL-1 mRNA and protein are under potent homeostatic inhibitory control by the hypothalamic-pituitary-adrenal axis (), the activity of which is increased by the activation of the 5-HT system ().
Collectively, the results of the studies reviewed suggest that the IL-1 and 5-HT systems engage in reciprocal interactions that contribute to the regulation of NREM sleep. In the POA/BF IL-1 enhances axonal 5-HT release and 5-HT stimulates the synthesis of IL-1, which inhibits wake-promoting neurons. IL-1 also inhibits wake-active serotonergic cell bodies in the DRN. Thus, IL-1 exerts opposite effects on serotonergic cell bodies and axon terminals. These effects complement each other and they both contribute to the same functional outcome: the enhancement of NREM sleep.
Why is sleep altered during sickness?
Sleep is clearly adaptive and much effort has been directed at determining its functions,,,. As we have reviewed, sleep is altered during infection. Infection increases the concentrations of cytokines, including IL-1, and the release of neurotransmitters, including 5-HT, in the brain, and interactions between IL-1 and 5-HT contribute to the regulation of sleep. We are beginning to understand how infection induces these changes, but it remains unknown why sleep is altered during sickness. We propose that altered sleep during infection, as a component of the acute-phase response and sickness behaviour, promotes recovery.
Is there any evidence to support the hypothesis that altered sleep during infection is a determinant of clinical outcome? Although it did not directly test this hypothesis, at least one study suggests that this might indeed be the case. Toth and colleagues retrospectively analysed data derived from long-term studies of bacterial or fungal infection-induced alterations in sleep in rabbits. The authors calculated for each animal a cumulative sleep-quality score that reflected both the duration and the intensity of NREM sleep. This approach allowed stratification of the outcome on the basis of whether the animals had high or low sleep-quality scores (good sleep or poor sleep, respectively) during the course of the infection. These cumulative sleep-quality scores were then correlated with the infective dose of the pathogen, multiple clinical parameters and the outcome. Analyses revealed that the infective dose of the pathogen differed between animals, and animals that received a higher pathogen dose generally had low cumulative sleep-quality scores. This suggests that the sicker the animal, the more disrupted its sleep. However, and of importance to this discussion, there were individual differences in the fates of animals that received the same infective dose: animals that survived had higher sleep-quality scores than animals that died. Although — as with any study that reports associations — this study did not demonstrate causality, and although it has yet to be repeated, these data are consistent with the hypothesis that dynamic changes in sleep during infection aid recovery.
How might infection-induced alterations in sleep promote recovery? We propose that they facilitate the generation of fever. In this view it is fever that imparts survival value, and fever could not develop during infection if sleep architecture was not altered. This hypothesis is based on two extensive bodies of literature, one describing links between sleep and thermoregulation and the other indicating that fever is adaptive.
The regulation of body temperature is coupled to sleep: superimposed on the circadian rhythm of body and brain temperature are arousal state-dependent temperature changes (). For example, brain and body temperature decrease during NREM sleep; the longer and more consolidated the NREM-sleep episode, the greater the decrease in brain or body temperature, until the regulated asymptote is reached. By contrast, brain temperature increases rapidly during REM sleep,(). In addition, thermoregulation is dependent on the sleep-wake state; for example, shivering does not occur during REM sleep,.

Vertebrates and invertebrates develop fever in response to administration of pyrogens (fever inducers) or infection with pathogens. Data demonstrate increased survival when the host develops a moderate fever during bacterial or viral infections. The survival value of fever to the host organism is conferred primarily by two mechanisms: facets of immune responses are potentiated at elevated body temperature, and the host environment is directly altered such that conditions for replication of the pathogen become less optimal,().

However, fever is energetically demanding: metabolism must be increased to raise and then maintain body temperature. It has been estimated that the mean increase in metabolism is 13% for every 1°C increase in body temperature. Increasing the amount of time spent in NREM sleep reduces the energy expenditure that is associated with competing activities, such as locomotion. But the changes in sleep architecture that occur during infection (suppressed REM sleep and increased but more fragmented NREM sleep) might have additional, fever-promoting benefits: shivering is crucial to the generation of fever but does not occur during REM sleep. Perhaps for this reason REM sleep is eliminated during the early stages of fever (). Furthermore, thermoregulatory mechanisms that reduce heat loss complement those involved in heat production (shivering) in the effort to increase body temperature. As heat dissipation normally occurs during NREM sleep, the fragmented nature of NREM sleep during the febrile response () may be viewed as a mechanism to reduce heat loss.
Data demonstrate that fever is adaptive and has evolved to increase survival in response to infection. Although it is unlikely that sleep has evolved solely to support the generation of fever during infection, the alterations in sleep in response to microbial pathogens are exquisitely designed to fulfil this role: the increase in NREM sleep conserves energy; the suppression of REM sleep allows shivering and, therefore, the production of fever; and the fragmentation of NREM sleep reduces heat loss.
Conclusions and future directions
Sleep is necessary for health as its loss or restriction is associated with multiple detrimental consequences. Although the interactions with neurotransmitters and neuromodulators through which cytokines enhance NREM sleep have been investigated at length, direct actions of cytokines on neurons in brain regions involved in the regulation of this sleep phase have only recently been determined. At present we know little about the mechanisms by which cytokines inhibit REM sleep. Investigating these mechanisms is important because REM sleep is disrupted in many pathologies that involve altered cytokine concentrations. For example, disturbed REM sleep and cytokine dysregulation are characteristic of major depression. In addition to elucidating the mechanisms by which cytokines contribute to the regulation of the amount, pattern and distribution of sleep, crucial functional questions also wait to be answered. More systematic studies are required before we can understand the nature of cytokine involvement in altered sleep during sickness. Also of importance is the question of the extent to which alterations in sleep during sickness contribute to clinical outcome. Do alterations in sleep during infection contribute to survival as we propose and as is suggested by correlations between sleep quality and survival of infected rabbits? Would recovery be facilitated if patients in hospitals were able to sleep better? Further investigation is required to better assess the mechanistic and functional relationships between sleep and morbidity and mortality, and to determine whether altered sleep promotes recovery.

Human immune system during sleep
A joint function of tissues, organs and cells for the protection of body develops immune system. The human immune response against various infections during sleep, its mechanism, neuroimmune interactions, immunoregulatory effect of sleep along with sleep deprivation and role of cytokines in sleep deprivation are addressed here.
Human immune system and sleep both are associated and influenced by each other. Sleep deprivation makes a living body susceptible to many infectious agents. In the result, immune system of human body is altered by releasing immunomodulators in the response of infections as reported by various researchers. The current situation requires improved sleep habits to make immune system efficient for a healthy life.
Introduction
Sleep is a physiological process that shows recuperative and regulatory characteristics. Immune system response is regulated by three physiological events such as
- Wakefulness.
- Non-rapid eye movement that is NREM or slow sleep
- Rapid eye movement that is REM sleep.
Various pathogens constantly attack living organisms, and the immune system which is composed of complicated networks of physical and biochemical components keep the organism existent .
In the 1970’s, the association between sleep and the immune system was first recognized when muramyl peptide acquired from bacterial peptidoglycan or Factor S from human urine was isolated chemically as sleep inducing factor . Immunoregulatory cytokine, i.e. interleukin (IL)-1, a key player in sleep regulation has levels associated with sleep propensity in the brain induced by muramyl dipeptide and Factor S related peptidoglycans. So, it is expedient that sleep regulated cytokines effect the immune system.
In a similar manner, inflammatory mediators increase due to constant sleep loss that alter CNS processes and behavior during immune feedback to infection, including sleep. Thus, during the intense phase response to infection or in chronic inflammation regulatory molecules cytokines are shared by sleep and the immune system involve in both physiological and disturbed sleep phase.
Human immune response against various infections during sleep, immunoregulatory effect of sleep along with sleep deprivation and role of cytokines in sleep regulation is discussed here.
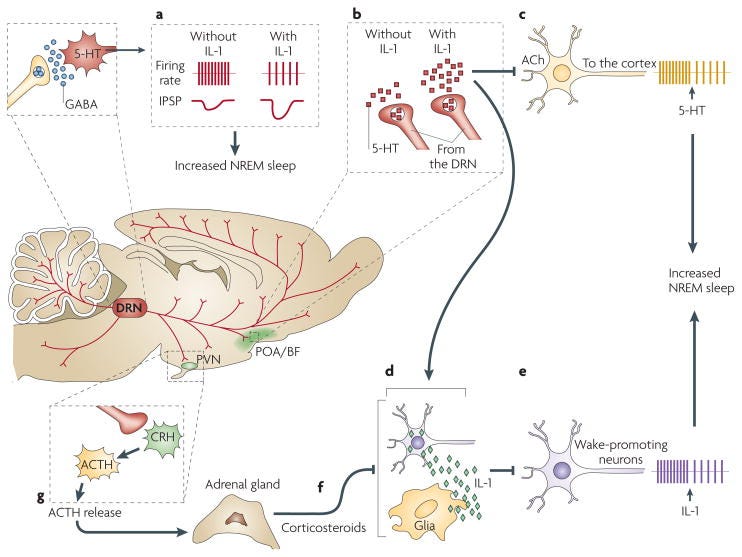
Mechanism of adaptive immune response supported by sleep
Fragments of antigen are presented to T helper (Th) cells along with the two types of cells which are involved in the formation of immunological synapse by APC that are antigen presenting cells that may pick and process invading antigen. Th1 response is induced by natural release of interleukin (IL)-12 APC and the function of antigen specific cytotoxic T cells along the production of antibodies by B-cells is supported by it as shown in .
Neuroimmune interactions
Particular anatomical and physiological conditions are based upon neuroimmune interactions whereas chemokines and modulators, cytokines and neurotransmitters, hormones are intercellular signals that may be shared by immune cells, neurons and glia cells . In both directions, blood-brain barrier can be crossed by some of the shared signals . In cerebrospinal fluid, nerve endings and at meningeal borders immune cells come in their close contact and flow in all directions throughout the body .
Somehow, sensory nerve fibers, sympathetic and peptidergic may also create connections between primary lymphatic tissues that are bone marrow and thymus and secondary lymphatic tissues such as lymph nodes and spleen. Immune functions not only be regulated by autonomous and endocrine nervous system through hormones and neural innervations but also through lymph flow, blood pressure and blood flow , oxygen, fatty acids and via supply of substrates like glucose .
Poor sleep and health
Downturn in activity and vigilance is not only indicated by sleep deprivation but it is an integral process that restrains many physiological functions.
Our capacity to remain healthy is badly effected by loss of sleep and sense of comfort, physiological framework accompanied by health is badly influenced by poor sleep . Our demand for sleep is also increased in most of the ailments as observed . Perceptivity to infectious diseases and deterioration of systemic circulation of leukocytes is increased by petty alterations due to lack of sleep . However, there is a huge complexity in both the immune system and sleep .
Infections, infectious diseases and immune system response
CNS is tainted by infectious diseases related to sleep disorders under the immune response against the infection whereas other systems like respiratory and endocrine systems are also affected by sleep disruption .
Virus as infectious agent
Immunodeficiency virus that is HIV and influenza are caused by viruses . Despite of declining body temperature, rapid eye movement sleep (REM), is decreased and non-rapid eye movement sleep (NREM) is increased by influenza virus leading towards fever, fatigue and sleep disturbances . Thus, temperature such as fever is increased in response to an infection to kill the cells causing the sickness as defense tool of body .
Bacteria as infectious agent
The whole functioning of the body is extremely altered in response to bacteria that cause diseases . In humans waking and REM sleep along with greater non-REM sleep is declined by Salmonella abortus endotoxin considerably. Thus, waking and sleep discontinuation with daytime drowsiness is enhanced by reducing the total duration of NREM by Salmonella abortus endotoxin.
Parasite as infectious agent
Sleep patterns and transformations of some behaviors are changed to promote parasitic infection and complete their life cycle . Transformation from wakefulness to REM sleep is baptized as sleeping sickness by Human African Trypanosomiasis HAT that effects sleep framework and nervous system to cause circadian rhythm dysfunction. Whereas a long time sleep leads to the less extent of parasitic infection and the sleep is developed to secure humans from parasitic infections .
Sleep deprivation and immunoregulatory effect of sleep
In case of severe and persistent loss of sleep such as insomnia, alcoholism, stress and during the period of aging, balance of cytokine is shifted from type 1 to type 2 leading towards type 2 function . In all these groups pro-inflammatory cytokines are enhanced constantly.
Ascetic alcoholics and people with less deprivation of sleep have high levels of TNF-α and IL-6 whereas tumor necrosis factor cytokine (TNF-α) levels are compared to control in sleep narcoleptics and apneics. T-helper (CD3+, CD4+), T-cytotoxic (CD8+) cell numbers and decreased natural killer (NK) cell activity is reduced in insomniacs along with elevated levels of inflammatory cytokines . Whereas daily framework of cellular and immune events cause to decrease overall immune functions in normal adults by experimentally induced sleep loss .
There is an inhibitory effect on hypothalamic pituitary adrenal HPA axis due to deep sleep in comparison to the HPA axis activation or organization of glucocorticoids which leads to arousal and sleeplessness . So, 24-hours increment in corticotropin and cortisol secretion, most frequent disorder insomnia along with a CNS hyperarousal disorder is caused .
Glucocorticoid and catecholamine plasma levels are increased for HPA axis activation clearly associated with lack of sleep due to removal of parasympathetic constituent of NREM sleep . So, in the morning after a night of sleep loss, fluctuated level of activation and normal level of cortisol becomes noticeable .
Role of cytokines in sleep regulation
A benchmark to be accomplished for a supposed sleep regulatory molecule is inducing physiological sleep along with its receptors in the living entity that fluctuate with the circadian rhythm or inactivation of the substance or its receptor cause to reduce voluntary sleep.
This criterion is fulfilled by cytokines as immune mediators as they are versatile proteins and they are involved in different physiological and pathological mechanisms in the CNS along with immune response .
Sleep proneness is associated with IL-1 levels in the brain, being highest at sleep onset, along cytokines such as IL-2, IL-6, IL-8, IL-15 and IL-18 are reported to increase NREM sleep whereas some proinflammatory cytokines manage physiologic body temperature and inclination . Best established cytokines are IL-4 and IL-10 and cytokines that cause discontinuity in NREM sleep are less observed and the production of IL-1 and TNF-α is restricted by inhibiting nuclear factor kappa-light-chain-enhancer of activated B cells (NF κB) activation by the activity of these cytokines.
Conclusion and recommendations
Communication network between the neuroendocrine and immune systems allows the body to maintain homeostasis, especially when it has to respond to a stimulus, such as an infection. The metabolic functions of the body to eradicate the pathogen are transformed during an infection. However, the brain mechanisms of sleep and the immune response are not completely figured out.
Generally, the effects of immune modulators cytokines, the sleep mechanisms, the resulting changes in the sleep-wake cycle and the effect of neurotransmitters in regulating sleep during an immune response are the processes which are associated. Subsequent studies reported that sleep deprivation decreases lymphocyte blastogenesis, NK cell activity and upregulates IL-1 and IL-2.
Furthermore, extensive surveys, search of literature and research on sleep patterns and their alterness during illness including novel approach to the mechanisms of cytokines, their receptors and role in immune system of human body is required.
Sleep and Health: Role of Dopamine
Introduction
Sleep is an important part of people’s lives and proper sleep is a prerequisite for good health. People have a need for a steady sleeping period of about 7–8 hours, especially during the night.
The reasons that gave rise to the need for sleep and the way the sleep was incorporated into the biological cycle are one of the great mysteries of evolution. The only thing we know for sure is that our sleep is necessary in order to be able to work during the day, so its disorder in any way adversely affects our everyday lives. Physical, mental and social well-being, as well as protection from certain illnesses and accidents, depends on the quality and the quantity of sleep.
Sleep, therefore, is a basic necessity of the human body and at the same time a basic prerequisite of its good health, in order its normal functions to be carried out. As a result, any sleep disorder has a direct impact on the body function, reducing its performance .
Recognizing the significance of sleep for the human’s health, the World Health Organization introduced 21st of March as World Sleep Day .
Normal sleep
Sleep is described as a special state of consciousness. It is composed of phases and is characterized as relatively unresponsive to the surrounding area. It is a periodic situation. The fall of consciousness during sleep provides time for the body systems to be reconstructed and renewed. Thus, sleep is a corrective mechanism that contributes to the regeneration of the person’s normal and emotional state. It occurs cyclically, usually once a day. Sleep is divided into two types, known as REM (Rapid Eye Movement), and NREM (Non Rapid Eye Movement)
NEM sleep is referred to as calm sleep and its awakening becomes more difficult. It passes from four phases. In the second type, we distinguish four (4) additional phases, which follow a specific repeating pattern throughout its duration .
- Phase 1: The first phase is subjectively considered to be lighter than the others and is often seen as a transition from the state of alertness to sleep. The person wakes up much more easily, the heart and respiratory rate falls slightly. At this stage a progressive muscle relaxation takes place, the body deeply sinks into an unconsciousness stage and faint images associated with the world of dreams are apparent. Electroencephalographic waves are observed similar to those observed during wakefulness (alpha waves with a frequency of 9–12 cycles) .
- Phase 2: The second phase is characterized by light sleep. The heart and respiratory rate is decreasing, body temperature and metabolism are decreasing. The second phase lasts about 10–20 min and includes 50–55% of total sleep. The eyes begin to turn around slowly. The slightest noise can wake the sleeper. It is distinguished by an encephalogram showing the characteristic groups of cells called sleeping spindles.
- Phase 3: The third phase marks the onset of deep sleep. The person wakes up with difficulty and rarely moves. It takes about 15–30 min and includes 10% of our sleep time. Heart rate, blood pressure and body temperature are decreased. Beta waves (a frequency of a wave per second and five times wider than alpha waves) occur in the electroencephalogram .
- Phase 4: The fourth phase is characterized by deep sleep. The heart and respiratory rate falls to 20–30% lower than that of wakefulness. This phase lasts about 15–30 min and occupies 10% of sleep time. The person is quite loose, rarely moving and difficult to awaken. Blood pressure, heart rate and body temperature have reached the lowest values. It is said that this phase promotes the physical state of man. Delta waves appear in the encephalogram .
Every night, when the person is getting ready for sleep, the body temperature decreases, the breathing becomes slower, the muscles relax and the person begins to yawn. The yawning is a prolonged breath and acts as a protective device to provide the body with oxygen when a fall in breathing occurs during sleep.
After the pre-mentioned four phases (in the meantime, almost ninety (90) minutes have elapsed since the person fell asleep), suddenly in the encephalogram there is a completely different phase from the previous ones. Alpha waves reappear, and the brain suddenly has a great activity as if awake. Circulation and temperature are increased. Diagrams showing the activity of eye bulbs (called nystagmograms) show a significant effect. It is what is called the REM phase, the phase of traditional sleep, where dreams appear . The person in this period turns to bed. During the night, each person usually dreams 90 min, divided into 5–6 phases of REM. The duration of this special phase tends to increase during the night. So the first phase, which generally appears around at midnight lasts 6–10 min, and the last, about 5 in the morning, lasts about 20 min .
REM sleep is referred to as paradoxical or active sleep. During it, effects from the sympathetic nervous system prevail. It is said that this type of sleep restores the individual’s mental state, in particular the functions related to learning, psychological adaptation and memory. It reviews processes and events that happened during the day, as well as other accumulated information .
The body seems to be paralyzed while the temperature, blood flow and oxygen consumption in the brain is increased. Moreover, heart rhythm, blood pressure and heart rate are elevated, the levels of which touch those of wakefulness. The rate of breathing varies from very fast, to very slow with periods of apnea .
In particular, REM sleep and the 4th phase NREM are of particular interest. Selective loss of either or both types of sleep creates need for replenishment. Thus, the body the next night increases the percentage of sleep and covers the gaps. This process is called replenishment phenomenon (Rebound effect) .
The body function presents daily high and low periods of physical and mental activity, which is determined by the so-called biological clock or circadian rhythm. The fact that man performs his duties during the day and night is asleep, suggesting that the biological clock initially is synchronized with the natural environment .
The body function presents daily high and low periods of physical and mental activity, which is determined by the so-called biological clock or circadian rhythm. The fact that man performs his duties during the day and during the night is asleep, suggests that the biological clock is initially synchronized with the natural environment .
The biological rhythm of sleep is often synchronized with other body functions, such as changes in body temperature associated with sleep patterns. The maximum body temperature value occurs normally in the afternoon, decreases progressively and falls sharply as soon as the person falls asleep .
The typical total length of 24-hour sleeping time varies 10 times between the species from about 2 hours in the giraffe to 20 hours in the small brown bat, while in humans it lasts about 8 hours. Nighttime sleep usually occurs in humans and many other mammals, but in some mammals occurs during the light period, as in rodents .
All people are asleep, although everyone has different behaviors in sleep. Some people need about 7.5 hours to rest and others need less or more sleeping hours. Younger people require more sleep than older people. As long as a person stays awake, the faster he wants to fall asleep. People are usually sleeping supine and having their eyes closed. This is not the case in some mammals that sleep with their eyes open, like the ox. Moreover, others sleep while hanging their limbs, like the bat, and others while standing, like horses .
The movement during sleep is relative. Some people during sleep walk or speak and the fish swim. In general, the response to endogenous and exogenous stimuli, decreases, is not removed, and this condition is reversible. Response to stimuli and reversibility are two characteristics that clearly differentiate sleep from death, coma and narcosis .
Sleep is also connected with a variety of physiological changes associated with breathing, heart function, muscle tone, temperature, hormone secretion and blood pressure. Data from various studies have shown that from 4 am, body temperature, blood pressure, plasma cortisol concentrations and adrenaline increase in order to prepare the individuals, when they wake up, to be ready for activity. The opposite happens as the night approaches. Plasma cortisol concentrations, mental processes and body temperature are progressively reduced to prepare the individual for sleep.
Utility of sleep
Sleep thus is a charging of our body’s batteries so that we can cope with everyday life having new forces. The importance of sleep in maintaining our body is also confirmed by serious disturbances that are caused when we do not sleep. As regards the importance of sleep, there is no longer any doubt that proper sleep is essential to good health. Physical, mental and social well-being, as well as protection from certain illnesses and accidents, depends on the quality and quantity of sleep .
Night sleep should be no less than 6 hours and more than 9 hours. As for the quality of sleep, which is function of the occurrence time and the relaxing effect, it depends on the lack of noise, the appropriate temperature, light meals and physical exercise. The comfort and stability of the sleeping area, as well as the observance of regular hours, also regulates the smooth functioning of sleep. This amazing sleep function seems to fulfill two functions, neurobiological and psychological .
The first is associated with the excretion of waste products of metabolic processes, the possibility of curing the CNS, especially in neonates and premature, by eliminating a large number of nervous stimuli bombarding the brain every day. The second is, according to Freud, a feigned satisfaction of our desires, and allows the vengeful and destructive loads to be neutralized, allowing the processing of a particular thought with consequent better acclimatization in real life. By performing these two functions, we are able to overcome intact the stimuli that usually bombard us . In addition to night sleep, human health is also affected by the habit of sleeping during the day, also known as siesta. This sleep is usually short-term, mostly common at midday hours, approximately 12 hours after the nadir of normal wakefulness .
Lunchtime sleep (siesta) is common in countries near the equator due to climate. It is also observed when there is a night sleep deficit, like in cultures and societies where dinner is taken late at night, night sleeping does not take place before midnight, and getting up from the bed is early in the morning. Daytime sleep is also observed in shift workers, those with hypersomnia, and in the elderly . Short sleep during the day has been associated with better health levels. However, in some people this habit may have negative effects, causing difficulties in night difficulties in night sleep and delayed alertness during afternoon awakening .
Factors affecting sleep
Many and various factors can affect and change the type of sleep, such as the following :
- General factors: Various life events such as noisy entertainments, intensive exercises, examinations in school or other trials, stress or stress from pressing work, etc. are included. All the above mentioned factors can change the type of sleep quantitatively and qualitatively.
- Changes in sleep can also be caused by environmental causes such as bed and sleeping changes, ventilation, lighting, or noise .
- Underlying disease: In a large number of diseases it is possible to observe changes in the type and amount of sleep. For example, conditions characterized by pain affect the person’s mood for sleeping. Nocturia, a common symptom for the elderly, can change the type of sleep. But also arterial hypertension often causes morning awakening, accompanied by a feeling of fatigue .
- The symptoms of people with duo dental ulcer are exacerbated due to increased gastric secretions during sleep. A large number of respiratory illnesses are also involved with sleep. Additionally, the intake of certain substances can alter the behavior of sleep. L-Tryptophan is a very basic amino acid which is found in a wide variety of foods. It is believed that it reduces the onset of sleep time. Due to this property, it was considered a natural hypnotic. Moreover, man’s habit of drinking a glass of warm milk before bedtime has a scientific basis, because milk contains this amino acid.
- Medicines: The effects and side effects of medications bring about changes in sleep. Indicatively, antihypertensive and diuretics are mentioned. The side effects of administering antihistamines and antihypertensive drugs are drowsiness, night-time awakening and gait. Their beneficial effect compensates for the side effects, which can be reduced either by developing tolerance or by choosing antihistamine that has fewer side effects than the reported ones .
- Sedatives, antidepressants and barbiturates also suppress sleep and their effects on sleep are quite similar to those observed in alcohol. From both causes, the latency of sleep time is reduced, continuous sleep and total sleep time increases and during acute drug administration, mild suppression of REM sleep appears. Very few of them promote sleep and this happens for a very short time .
- Changes in sleep may be caused by many drug and substance groups, such as alcohol, anticholinergics, anticonvulsants, antidepressants, antihistamines, opiates, stimulants or irritants, and opioids.
- Antidepressant drugs may change the type of sleep indirectly due to underlying depression, which causes sleeping abnormalities and directly due to the drug effect on sleep. The most persistent effects of antidepressant drugs on sleep are the general suppression of REM sleep and the prolonged latency of REM sleep. Sudden discontinuation of antidepressant drugs can lead to a prolonged period of REM sleep replacement, and the person usually complains about tension, dread and reduction of sleep quality.
Sleep deprivation
Well-documented studies report that after 10 or 20 hours of insomnia, signs of excessive fatigue, reddening of the eyes, some mistakes in perception are beginning to appear. We have the illusion that the floor waves. There is a substance in the blood, the in dole, which belongs to the same family as the hallucinogen L.S.D.
If an individual stays sleepless for 60 hours, he will experience symptoms such as reduction of neck reflex, hand tremor, nystagmus, clumsy movements, eyelid dropping, dysarthria, difficulty in concentrating, reduced facial movements, and his general appearance seems to be apathetic. The changes start on the third day with illusions and as the sleep deprivation continues, perceptual, cognitive and psychomotor capacity of the individual are reduced, while visual hallucinations appear .
After 90 hours of insomnia, we have the impression that our face is full of spiders and it is impossible to distinguish between dream and reality. The electroencephalogram reveals the presence of a “short-sighted” period, where the person, although awake, has the same cerebrovascular features of sleep (slow waves). An individual under these conditions becomes a real public danger and can respond with reactions totally disproportionate to insignificant things.
Recovery from sleep deprivation is accompanied by increased overall sleep time. The values of the amount and type of the different sleep phases are restored during the first night of recovery.
Sleep disorders
Sleep disorders affect not only sleep but also many more aspects of life. They are related to adverse effects on the quality of life and health status during the day. There are three (3) main types of sleep disorders related to the biological sleep clock :
- Type of delay of the sleep phase: The person cannot move the time of sleep and wakes up earlier than usual, so he sleeps and wakes up slowly in relation to the existed social requirements. People with delayed sleep phase often report that they feel sleepy in the early hours but are more energetic and alert late in the evening .
- Jet lag type: The cycle of sleep and activity for most people is synchronized with the pace of day and night at the geographical point where they live and work. Jet lag is due to the de-synchronization between the various rhythms of the organism and the environmental rhythms. The rhythm that is most affected is the cycle of sleep and activity, with the associated changes in physical and mental functions. Symptoms of this syndrome are somnolence, fatigue, difficulty of concentrating, and irritation during the day. People, despite their fatigue throughout the day, cannot sleep and their sleep is anxious. This syndrome resolves in 2–7 days, depending on the travel distance from east to west and temperamental sensitivity .
- Many people think they can avoid symptoms by changing eating and sleeping times before traveling. Others also think that the onset of the syndrome is directly related to lack of sleep, so sleep is the solution itself. Special treatment is not required .
- Type of shift change: This disorder is due to people working on night shifts or frequent shift changes. Shifts disrupt the worker’s biological rhythm. Rolling working time creates short- and long-term health effects. Effects include sleep disorders, cardiovascular disease, gastrointestinal disturbances and aggravation of chronic conditions. Young people and teenagers tolerate rolling schedule, showing fewer symptoms than the elderly . It accounts for 10% of shift workers, which necessarily include night shifts. People’s sensitivity to program changes varies widely, and a respected number of people simply do not adapt to changing hours. These people should not be employed on such a timetable. In this case, things are therapeutically more complex, because it is not always easy to change the individual’s job. This is a medication that induces vigilance 30–60 min before the job, which is combined with the treatment of insomnia that occurs when the person wishes to sleep during the day .
Effects of sleep disorders
Sleep disorders can have serious effects on memory, learning, cardiovascular, nervous system, reduced productivity, our social behavior, and general deterioration in quality of life .
Sleep and diseases
To a large number of diseases, changes in the type and amount of sleep may occur. For example, conditions characterized by pain affect the person’s mood for sleeping .
4.2.1. Sleep in Parkinson’s disease
Parkinson’s disease is an age-related disorder characterized by movement disorders such as stiffness of the body, slowing of movement, and trembling of limbs when they are not in use. In advanced stages it progresses to dementia and eventually death . The main symptoms are caused by the loss of dopamine-secreting cells in the substantia nigra .
More than 96% of patients suffering from Parkinson will experience sleep disturbances during the course of the disease. They are due to the interaction of various factors, such as motor problems (stiffness), circadian rhythm changes in sleep-wake cycle, behavioral disorders in sleep REM, psychiatric problems (anxiety, depression, dementia), side effects of drugs. It should be noted that the treatment of Parkinson’s disease among its side effects includes sleep disorders characterized by daytime sleepiness .
Apart from the breakdown of nighttime sleep of the reported causes, 15% of patients with Parkinson will develop sleepiness throughout the day during the course of the disease. It is a sudden advent of sleep, in an inappropriate environment, without warning and without the possibility of suspension. Daytime sleepiness may be due either to the progression of the disease or to the various disorders that interrupt nighttime sleep or to the side effects of anti-Parkinsonian drugs .
Regarding the treatment of sleep disorders in Parkinson’s disease, it aims to treat each individual disorder separately. In each case it is personalized. The basic principle of treatment is not to use plethora of sedative and hypnotic drugs. The medication is aimed at regulating anti-Parkinsonian treatment to reduce the kinetic problems that disturb sleep .
Dopamine is an organic chemical that plays several important roles in the brain and body. Also it is an amine synthesized which is synthesized in the brain and kidneys. Therefore in the brain, dopamine functions as a neurotransmitter and send signals to other nerve cells. The brain includes several distinct dopamine pathways, one of them plays a major role in the motivational component of reward-motivated behavior .
In particular, dopamine is an organic substance used by nerve cells to communicate with each other. Dopamine acts on receptors found in the immune system cells and all dopamine receptor subtypes are found in lymphocytes. Several diseases have been found to be associated with damage to dopamine system. Dopamine deficiency caused by Parkinson’s disease is associated with reduced movement, fatigue, slowing or blurring of cognitive functions, stiffness, loss of initiative or mobilization, and aggressive behavior in competitive situations .
Dopamine is available as an intravenous drug that acts on the sympathetic nervous system, with an increase in heart rate and blood pressure. However, due to the fact that dopamine cannot cross the blood-brain barrier, dopamine given as a drug does not directly affect the central nervous system. To increase the amount of dopamine in the brain of patients with conditions such as Parkinson’s disease and dystonia, L-DOPA (which is the dopamine precursor) is often prescribed, because it crosses the blood-brain barrier . Although L-DOPA treatment cannot restore the dopamine cells that have been lost, but it causes the remaining cells to produce more dopamine, thereby compensating for the loss to at least some degree .
Some medications act as dopamine agonists and can treat its low levels (hypodopaminergic) as they are typically used to treat PD, attention deficit disorder, hyperactivity disorder, certain mucosal tumors (prolactinoma), and they can also be useful to restless legs syndrome (RLS) . For the treatment of Parkinsonism drugs such as bromocriptine and pergolide are sometimes used, but in most cases L-DOPA appears to give the best trade-off between positive effects and negative side-effects . The development of a dopamine dysregulation syndrome is sometimes associated with dopaminergic medications, which involves the overuse of dopaminergic medication and medication-induced compulsive engagement in natural rewards like gambling and sexual activity .
Restless legs syndrome (RLS) is a common sensory-kinetic disorder characterized by abnormal sensations that appear initially at rest or during sleep, relieved by the movement of the affected limb. The pathophysiology of RLS remains unclear although the role of dopamine dysfunction and iron deficiency in the brain, have been suggested .
Symptoms include unpleasant sensations in the extremities, especially in tibia. They can appear on both legs, sometimes also offend the hands. Individuals who have the syndrome usually report symptoms described as chills, tingling, burning, pain, pulling or even as something creeping under the skin. Symptoms get worse when the patient rests and they are improved with the movement. Symptoms are usually getting worse in the evening and during the night, so these patients often have poor sleep quality and consequently often experience daytime sleepiness. It is noted that there is no cure for this syndrome .
Treatment with dopaminergic agonists relieves symptoms, but does not result in total healing . Adherence to the hygiene rules of sleep is also important. At the same time, psychiatric help is sought if the disorder is due to a psychiatric problem .
It is also noted that Researchers from the University of Barcelona and the Centro de Investigacion Biomedica en Red de Enfermedades Neurodegenerativas (CIBERNED) in Spain has discovered a new function of the neurotransmitter dopamine in controlling sleep regulation. The act of Dopamine in the pineal gland is central to dictating the ‘circadian rhythm’ in humans — the series of biological processes that enables brain activity to adapt to the time of the day . The translation of the light signals from the pineal gland which is received by the retina into a language understandable to the rest of the body . In conclusion, the formation of these heteromers is an effective mechanism to stop melatonin production when the day begins and to ‘wake up’ the brain. This new function of dopamine could be extremely useful when designing new treatments to help mitigate circadian rhythm disturbances, for example those related to jet lag, those found among people who work at night, and in cases of sleep disorders in general .
Obstructive sleep apnea and diabetes mellitus
Most patients with diabetes mellitus (SC) have insufficient sleep in duration and quality. On the other hand, short-term and poor-quality sleep seems to adversely affect glucose metabolism and is associated with an increased risk of developing AD1.
Patients with diabetes mellitus (SC) suffer from obstructive sleep apnea very often. It is likely that AD increases the risk for development of obstructive sleep apnea, mainly through the mechanisms of inflammation and autonomic nervous system (ADN) dysfunction. Additionally, diabetic neuropathy is associated with increased sensibility of promectal chemoreceptors to CO2, and sensitivity of peripheral chemoreceptors decreases .
Obstructive sleep apnea syndrome (OSAS) is a disorder that is characterized by repetitive partial or complete closure of upper airway during sleep. Also, obesity is the most important risk factor for OSAS. Many case studies in the literature show that OSAS is associated with insulin resistance, glucose intolerance and type 2 diabetes, independently of shared risk factors .
Sleep in chronic kidney failure
Sleep disturbances are very common in patients with chronic kidney deficiency. Pathophysiology is complicated and may include a combination of factors such as fluid balance, anemia, cardiovascular function, concomitant diseases, medications, physique, psychosocial and demographic factors and everyday habits. Recognition and treatment of these disorders can improve the quality of life and reduce morbidity and mortality in this patient .
The most commonly reported complaints are insomnia, Restless Legs Syndrome, sleep apnea and excessive daytime sleepiness :
Sleep and age
Age plays an important role in sleep duration as well as the formation of its internal architecture. As a person grows up, average sleep time falls from 16 to 18 hours for infants to 8 hours for a 12-year old child, then 7.5 hours for people between 25 and 45 and 6.5 hours for the elderly. Alongside with age, two things increase: the latent time that sleep comes and alertness time after sleep begins, that is more awakenings and inability to sleep again take place .
5.1. Sleep during infancy
During the first weeks of the infant’s life, awakening at regular times during day and night is considered completely normal. Infants usually sleep all day with few intervals. The sleep-awakening cycle includes sleep and waking up for feeding and diaper change. Infants usually have an irregular such cycle and sleep 10–18 hours a day . In order to develop the right models of sleep, babies have to go to bed when they feel sleepy and not when they are already asleep. Moreover, they have to learn to sleep by themselves from their first months. At the same time exposure to the sun and playing under it can guarantee a quieter sleep at night. A baby’s sleep gets more normal from the 4th to the 6th month because later it gets more difficult. Sleep duration is determined by neurological maturation, temperament factors and the baby’s emotional state. When the baby has a troubled sleep, a sleep steady schedule needs to be followed .
The infant needs to sleep in specific hours during day and night, in a specific environment and with the following characteristics :
- In its cot or basket with a stable and not very soft mattress.
- Low lighting.
- With relaxing music over its bed.
- With one of the baby’s favorite dollies.
In the first 3–6 months, even if the baby has its own room, it is more practical for the cot to be in the parents’ bedroom, so that they can feed it as easily as possible. Room temperature needs to be between 18 and 22–23°C. Its pajamas have to be light, the bed linen to be a light feather or woolen duvet or sleeping bag in winter, and in summer a sheet or cotton blanket is enough .
If the baby finds it difficult to sleep at night then a series of specific actions before sleep take place, such as a bath, a tender hug, lullaby or kiss, so that the baby can connect sleep to a pleasant feeling and sleep faster.
When it wakes up and cries at night make sure to see if it is hungry or its diaper wet, so as to give it milk or change the diaper. If it is in colic pain, rub its belly with oil. When the first teeth start to grow, you can put some gel on its gums to relieve pain after consulting the doctor .
For infants up to 1 year old the ‘sudden infant death syndrome’ is the first cause of death. Diagnosis takes place after ruling out all other possible causes of death. Breathing or heartbeat problems during sleep could be partially the cause as well. Death comes after arterial pressure falls and heartbeat slows down gradually till it stops. Main risk factors include smoking or drug use by the mother during pregnancy and after labor, cold winter weather and a baby’s face-down position during sleep .
5.2. Sleep in children
Children’s sleep changes with age. Before the 3rd month of life they pass from alertness to sleep with REM sleep directly, whereas after their 3rd month with NREM, like adults. The REM sleep rate changes as well. For a newborn it is 50%, while gradually it falls to 20–25% until the child is 3 years old [ 65]. Normal sleep duration also changes with age. For newborns it is 16–18 hours, for infants 13–15, preschool age 12–13, school 11–12 and in adolescence 9 hours. Usual sleep start time in toddlers is 8–8:30 p.m., while for teenagers it is 11–11:30 .
Sleep is a vital part of children’s healthy development and is related to their physical, cognitive, emotional and social growth. In most cases sleep disorders are temporary, without long-term results. For some children, however, they can be very important .
In children sleepiness due to lack of sleep manifests as lack of attention, hyperactivity or aggressiveness. Lack of attention then has consequences on memory and learning. Quite often parents do not mention their child’s sleep problem to the pediatrician or do not see the relation between sleep disorders and behavior during daytime. Thus, in a routine visit to the doctor questions about sleep need to be asked .
In pre-school children parasomnias are common, for instance nightmares, talking through sleep or night terror. Their frequency gradually decreases during the first 10 years of life. Most common sleep disorders in children are .
Behavioristic insomnia
Two types of it are often present in the same child. In the first, the child resists verbally or postpones sleep claiming fear, or leaves the bed and goes to find the parents. If time is lost its sleep is inadequate. The second type is about continuous night awakenings. The child that is used to going to bed under certain circumstances, like feeding or rocking in parents’ arms, cannot calm down if it wakes up and cannot go back to sleep without the parents there.
Treating behavioristic insomnia: If all other medical problems are ruled out, like belly pain, breathlessness, otitis, allergic rhinitis, atopic dermatitis, underlying neurological disease or pharmaceutical effect, then the following measures are taken :
- Steady sleep routine, around the time pre-school children go to bed (around 8–8:30). This should start 20–45 min before desired sleeping and include a bath, clothes changing, story narration or a game or blanket.
- The child should be in bed before falling asleep and not after.
- For children who wake up at night ‘systematic indifference’ is followed, that is no help is given to sleep again at night, so as to eliminate the need for a parent to be present (graduated extinction).
- The parent leaves child’s room before it falls asleep. Every time it wakes up and looks for them, they have to wait more and more before answering.
- A positive behavior needs to be strengthened through reward.
Research shows that interventions in behavior clinically improve 80% of children to a great degree. No child showed any side effects from these treatments, and there is also a great secondary benefit in improving the daily behavior, self-confidence and mental health of the child and the parents .
5.2.2. Parasomnias
These are undesirable natural events or experiences that occur during sleep, during sleep or awakening. They are considered benign phenomenon in children and — if not very common and intense — they do not affect the duration and quality of sleep. They may exist individually in a child or co-exist with neurological psychiatric or other problems. Often there is a similar background to one of the parents .
The most common parasomnias in pre-school children are :
Treating parasomnias: It is usually enough for the parents to reassure the child or stay with him until the end of the episode, while using various behavioral techniques such as programmed awakening. Drug administration is limited to selected cases of very resistant forms or to children with severe neurodevelopment problems and is given for a short time .
5.2.3. Respiratory disorders in sleep
It is a range of disorders ranging from simple snoring to classic obstructive sleep apnea, sleep apnea, or central hyponatremia syndromes .
Moreover, 10–12% of children snore, but even this disorder, which is otherwise benign, may have neuropsychiatric effects such as more anxiety, attention deficit disorder, social problems and depression. The most frequent and most important of all respiratory disturbances of sleep is obstructive apnea. These are episodes of partial or complete obstruction at the air intake during sleep, resulting in a reduction in oxygen in the blood .
The most common causes are hypertrophic tonsils and adenoids (carnations), craniofacial abnormalities, obesity and neuromuscular diseases. These recurrent sleep obstructions often result in waking up and a decrease in deep and relaxing sleep. The child can snore, sleep with open mouth, and wake up often to get breath, sound like drowning, getting night terrors or enuresis, sleepwalk. During the day it presents drowsiness, distraction, reduced academic performance, hyperactivity, and over time may present hypertension . Depending on the underlying cause, obstructive sleep apnea is treated with weight loss, medication, surgery, even with sleeping apnea (CPAP) devices .
There is also a minority of cases that need to be investigated, such as when the child snores or has sleep apnea, presents secondary enuresis, and finally to exclude epilepsy. Seizures, especially nighttime spasms originating from the frontal lobe of the brain, may be misdiagnosed as parasomnias .
Particular features from the child’s history may help to distinguish. Convulsions occur at any time of the night, are stereotyped, shorter or occur several times the same night. When it is difficult to distinguish, further investigation by electroencephalography and polyp’s graphic study is recommended .
Moreover, narcolepsy, although considered unusual in children, is rather sub-diagnosed. It is a disorder characterized by chronic daytime sleepiness with sleeps episodes during the day (usually 3–5 episodes lasting 10–20 min) that occur more frequently during monotonous activity. Many adult patients with postnatal narcolepsy report having symptoms as children. Narcolepsy has a genetic basis, is a chronic disease and its treatment is only symptomatic .
Restless legs syndrome also in some children may be synonymous with “growth pains.” It is a hereditary disorder, usually a family history. This is a kinetic sleep disorder, in which the person complains about a strange, disturbing, creepy sensation on his feet, like something is crawling, appearing in the evening and at night. Some patients experience improvement by iron administration. This annoyance is temporarily relieved by the movement of the legs and so the person feels the need to shake his legs. This movement prevents him from falling asleep or breaking his sleep, resulting in fatigue and drowsiness in a day .
Sleep disturbances have a significant impact on the quality of life of the child and the family and are often treated easily. This underlines the need for proper diagnosis. Parents should monitor the sleeping of their children and when they recognize an unusual sleep behavior need to consult their pediatrician .
Sleep in the old age
When talking about sleep disorders in the elderly, we mean those that affect the ability to initiate and maintain sleep, including excessive sleep duration.
The timing and amount of sleep change with age. Elderly people tend to sleep early, wake up earlier and tolerate less changes in the sleep-wake cycle. As the circadian rhythm varies with age, fatigue tends to become more intense as the sleep time increases. When this happens, the person wakes up earlier and the cycle repeats itself. Sleep efficiency / sleep duration compared to bedtime, decreases from 95% during puberty to less than <75% during third age .
Restless sleep in the elderly is due to various factors. First of all, poor sleep hygiene habits. Also, a medical or mood disorder that is adversely affected by sleep is more likely to occur, and medications to treat them may cause sleep disturbances. In addition, the possibility of primary sleep disorders, such as sleep apnea that may aggravate disturbed sleep, is increasing. Finally, aging affects the functioning of the urinary bladder, circadian rhythm, or hormone secretion and body temperature. These factors may result in less rejuvenating and more disturbed sleep .
There are some age-related changes in sleep, although sleep disorders in the elderly may be related to psychological stress and stimuli, such as:
Sleep in the hospital
Sleep of the patient is a vital need and its fulfillment is a nursing responsibility. Only addressing the sleep problem requires not only specific scientific knowledge, as was said at the outset, but also a combination of nursing procedures in the context of integrated nursing care. Often, the patient does not have enough sleep, and this has an unpleasant effect on his psychosomatic well-being and resistance to the disease, as well as on health rehabilitation. In general, deprivation of sleep to a serious degree may cause disorder of thought and behavior, melancholy .
Preparing the patients for sleeping, ensuring adequate sleep and monitoring their condition at night are unique nursing responsibilities, as no other health care profession has this concern . For effective nursing care of sleeping patients, nurses need specialized knowledge from many sciences, including :
- The physiology of sleep.
- Sleep disturbances and pathology.
- The psychology of sleep.
- Pain and anxiety as causes of insomnia.
- The pharmacology of hypnotics.
- The theory of dreams.
- The nursing system, such as patient preparation for sleep, night care, etc.
- The art of communication, because with this the nurse will identify and solve the problems of the patient’s sleep.
- Technical nursing measures to ensure physical comfort.
As the most common causes of insomnia in the hospital environment are considered :
Surveys have also shown that the factors that disturb the sleep of patients include the following :
- Noise created by staff e.g. Conversations, book browses, and more.
- Noise and other environmental disturbances e.g. Squeaking doors and wheeled vehicles, sudden strikes of objects, cardio scopes, rewinders, suction fans, sliding furniture, telephones, intense lighting etc.
- Nursing and treatment procedures e.g. taking vital signs, injections, individual care.
- Noises generated by other patients, such as conversation, coughing, vomiting, snoring.
- The pathological condition of illness, pain, fever, discomfort, bedtime, lack of private space, difficulty in oral communication such as endotracheal intubation or aphasia, fear of death, and so on.
The patient struggling to sleep in so many noises reaches the point of wondering whether sleep is permitted in the hospital. Nurses again, as a health care professional, with their own personal interest, “good art” and their scientific education, have to care for the patient’s exercise, keeping them busy, rest and sleep; this must be the link, the true dimension of hospitalization .
More importantly, nurses’ responsibility in terms of sleep advancement is to help the person at all stages of the disease to ensure adequate, calm and effective sleep .
Information about the sleep environment is whether the person sleeps alone or shares the room with another, the number of pillows and bedding him uses ventilation, lighting and noise. Also noted are the drugs and the type they use, if they are eating before bedtime, the type of food and drink they are used to, whether they are showering or bathing before eating. In particular, the person’s views on rest and sleep time he considers necessary to operate at desired levels are considered .
- General nursing interventions
- Help the person recognize that he is exercising control over his type of sleep, and that he can achieve restful sleep by natural means such as noise avoidance, normal temperature, and reduced light.
- Help identify the type of sleep, sleeping habits and pre-sleep habits.
- Help distinguish or establish a type of sleep relaxing and comfortable for oneself.
- Encourage patient to identify the factors that affect his sleep pattern.
- Take leisure and activity types throughout the day, in the afternoon and in the evening when planning your nighttime sleep.
- Nursing interventions for daily program
- Encourage the person to actively participate in activities appropriate to his/her situation. Design rest periods and activity for the whole day.
- Help patients detect the time of daytime sleep. When the sleep of the day is taken at the same time and for a planned duration it is beneficial.
- Help to avoid frequent insomnia throughout the day. Serious sufferers and those undergoing surgery will have a greater number of short-term sleep during the day.
- Nursing night program interventions
- Help the person reduce their activities before bedtime.
- Encourage you to define and perform your pre-sleep habits and help them adapt to the hospital environment.
- Give a gentle rub, place a suitable bed, keep it dry and clean.
- Offer them the right reading or music.
- Know that stress is more common at night. Give opportunities to the sick person to talk to you about his interests and his fears. Suggest that he discuss it with a family member or a trusted friend of his.
- Include the painkiller in the patient’s program and administer it before bedtime. Although these drugs may affect the type of sleep, relief from pain is of greater importance.
- Plan hospitalizations so as not to disturb sleep, such as avoiding diuretic or stimulant administration before bedtime.
Conclusions
Sleep occupies about one third of our total lifetime and is a very important biological function. Its functional significance is related to the resting of brain function and to the proper functioning of memory and learning. Sleep deprivation causes disturbance of attention, performance at work and emotion.
Therefore, sleep is essential for a smooth living. Its duration is satisfactory when we wake up rested and rejuvenated. The duration of sleep differs from person to person but is estimated at about 8 hours a day. With aging, it usually reduces its duration and many elderly people sleep 5–6 hours a day.
In order to have a normal sleep, it is good to respect our biological clock that is to try to sleep for about the same hour at night and to wake up at about the same time in the morning.
